Before Dara started chemo I’d known plenty of people with cancer at a variety of ages. Other than understanding that chemo is extremely difficult and disabling, I didn’t know what was involved. Going through the chemo process with someone as girlfriend and primary caregiver has been an extremely different experience and there is a lot that I’ve learned. Helping to ease the discomfort of the person you love the most in the world is a huge motivator to suck up information like a sponge! I wrote the below for a friend who asked for a relative about to go through chemo and I thought it might be a helpful blog post. It’s long so I tried to create headers and bold stuff for easy reference. I’ll write more another post about my experience as a caregiver (I’ve learned a lot) and about the other parts of her treatment.
Dara’s experience with chemo hasn’t been consistent as side effects change and shift. Before she started her treatment everyone (doctors, nurses, former/current chemo patients and their caregivers) said that all bodies react differently to chemo and things will be somewhat unpredictable. Even all the research we did ahead of time wasn’t really helpful until she was actually going through the experience. This is an account just of one person’s experience with the physical and emotional affects of chemo as they’re happening.
She’s on a sixteen week course that consists of eight two week cycles for her Breast Cancer. The first four treatments were of Adriamycin/Cytoxan (abbreviated A/C) and the last four treatments are Taxol (abbreviated T). Different poisons that do different things but they both suck.
In case you don’t know how chemotherapy works, basically it treats cancer by stopping cells from being able to grow and divide—this affects both cancer cells and non cancerous cells. Since your hair follicles are some of your fastest reproducing cells this is why during chemo your hair might fall out.
Going into chemo Dara kept saying she’d heard chemo was “better than it had ever been” which, after I unscientifically polled my Facebook friends who have cancer experience, I think that statement just meant that the drugs to treat the side effects were better so folks experienced less terrible side effects. Also there are lots of different chemo treatments now that get better and better as cancer research comes out. I’ve learned a lot from the nurses we’ve hung out with during Dara’s infusions. Sometimes folks who used to have to be in the hospital to get their chemo infusions over a long period of time can take their chemo meds and go home with them for a 24 hour infusion. There’s a new treatment where folks just take a chemo pill and it isolates and blasts specific kinds of cancer cells without killing the other cells in the body.
During the Infusion
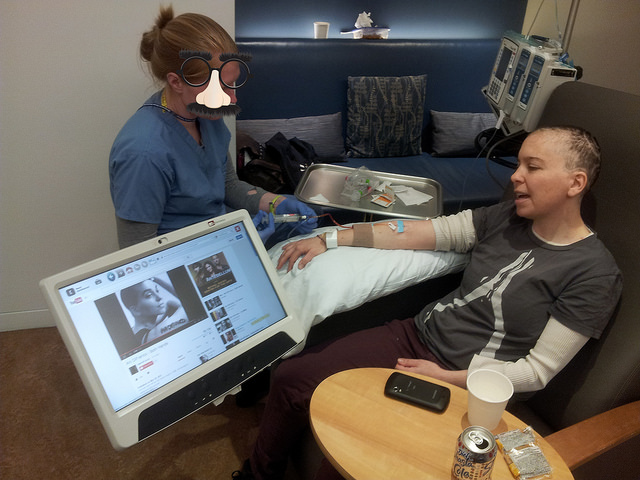 We were asked by the MSK publicity department to not include staff faces in a video Dara shot at her infusion center, so even though we heart everyone we work with there we’re keeping that up on our photos for the blog. Hence the “disguise” above.
We were asked by the MSK publicity department to not include staff faces in a video Dara shot at her infusion center, so even though we heart everyone we work with there we’re keeping that up on our photos for the blog. Hence the “disguise” above.
Dara’s actual chemo infusions are as close to fun as anything involving IV lines can be. The care she’s gotten at Memorial Sloan Kettering has been amazing. The nursing staff at the Brooklyn Infusion Center is incredibly kind, caring, smart as whips and fun. The infusion suites have recliners, a couch for the loved ones, these consoles with internet tv and games on them, free wifi, baller coffee machine and a pretty great fridge with shasta colas. I’ve had friends suggest bringing games and activities to chemo, and we’ve had a ball doing chemo karaoke when the actual chemo goes in. Bell Biv Devoe’s “Poison” and Alice Cooper’s “Poison” were on the first round playlist.
During the Taxol treatment she gets Benadryl as a pre-med (meds she gets before the infusion, along with IV steroids to help prevent nausea) so she spends that three hour infusion asleep and I do work on my laptop.
The day before her chemo infusion she goes in to see her oncologist and the practice nurse (the nurse who only deals with that doctor’s patients) to talk about the side effects and have a physical exam. She also gets lab work done and we sit down with the scheduler for all her upcoming medical appointments. This process is usually an hour and a half but with wait times can be up to three hours. The main campus of Memorial Sloan Kettering is on the Upper East Side, which is an hour each way for us. There’s free wifi and the good sodas there, too, which is helpful for me to get work done. I bring this up as part of the chemo process because sometimes the schlep and amount of doctor wait time affects how she is feeling and her ability to recover.
How Chemo Feels
Her first few weeks on chemo she was able to isolate “glory days” where she felt good for about the five last days of her cycle—almost back to normal in terms of energy. She says, “It might be better than normal because when you feel normal after feeling crappy for nine days you feel like Superman.” In the fourth cycle she didn’t really have “glory days” and then with the Taxol treatment it’s more like “glory hours” where for a few hours a day she’ll feel okay or have some energy but not reliably.
Feeling good during chemo has been affected by her period, which stubbornly hung on for awhile even though it surprised her doctors that she was still getting it. PMS plus chemo is basically the worst. She also thinks that anything else that was wrong with her before chemo has gotten heightened, like chronic lower back pain.
You Kinda Can’t Do a Lot During Chemo
There’s all kinds of things she can’t do other than the physical obvious stuff that she doesn’t have energy for. No vitamins other than Vitamin D because you don’t want to strengthen the cancer cells we’re trying to kill. No spirulina or other supplements. She was doing a bunch of anti-cancer diet stuff before chemo started and they told her no juicing more than 6 oz a day but she hasn’t been able to drink fresh juices since the nausea started. No tears or punctures to the skin as much as you can help it because you can’t heal that fast and therefore, infections. She had to switch to a soft toothbrush and even then her gums were bleeding like crazy for a couple of weeks.
Chemo makes you immune compromised, so she has to be wildly careful how she interacts with other people and hand washing/hand santizer is an all the time thing. Using hankies or scarves to open doors/touch elevator buttons, etc… Our chemo nurse Erin said that as much as possible learning to never touch your face is a really important way to prevent catching things. As caregiver I have to be extra careful to not get sick as well because if I’m sick she can’t be around me. We have to tell anyone who comes to visit to cancel if they feel that they might be sick or getting sick.
 You get used to seeing these masks during cancer treatment.
You get used to seeing these masks during cancer treatment.
She is given a shot of Neulasta the day after her chemo infusion (luckily this happens in Brooklyn as well) to encourage her bone marrow to produce more immune blah blah blah and she gets some bone pain from it. Her white blood cell count has been pretty high for awhile and then one week went up to 39 which was like enough WBC for everyone in the hallway we were in, as her doctor said, so they skipped it for one cycle. If the WBC is too high something goes wrong but I forget what doomsday thing they said. We had to go in for an extra round of labs the week after they skipped it to make sure she didn’t dip too low.
Hydration has had the hugest effect on her overall experience of side effects. She hated drinking water before chemo. We have done all sorts of things to encourage her to drink more. Coconut water is a huge help (she’ll go through a carton a day sometimes), I found all these calorie-free drink mixes that are meant for water bottles in my cabinet, tea, lemon in water, etc… We also do a daily chart marking off her water intake and I give her stars for a behavior chart every day she drinks all her water. Sometimes working towards a goal, especially when you don’t feel great, really helps.
Watching TV really helps, because it distracts her from her bodily discomforts. Sometimes when friends come for a visit she says, honestly, after a bit of chatting, “I really just need to watch TV now, want to watch with me?”
Feeling “high” from her drugs is not exciting for Dara. She doesn’t find it as fun when it’s high for a medical purpose than recreationally. Plus she wants to feel like she can function and it’s hard to decide to take a drug that makes her feel disconnected from everything around her. Sometimes it’s a welcome relief but most of the time she toughs it out rather than getting high.
The biggest side effects she’s experienced are fatigue, nausea, pain, constipation and extreme emotions. Nothing has been a slam dunk in terms of what’s helped ease them. Something helps for awhile and then maybe it doesn’t anymore, or the side effect gets different or worse.
Fatigue
She just gets tired. At first I thought the experience of being around her while on chemo was like having a partner who has the flu but since it’s not an all the time thing it’s just like BAM she gets tired, so maybe the flu for a few hours. Maybe 10% of the time she’ll get winded going from the living room to the bedroom. And 10% of the time she’s totally up at her normal capacity for running around. The other 80% is somewhere between those two extremes.
 Going to the park during her first “Glory Day”.
Going to the park during her first “Glory Day”.
Nausea
The anti-nausea meds work really well for some people and for Dara they weren’t great. She was extremely nauseous most days she was doing the A/C treatment. Luckily, the Taxol treatment is mostly about pain and not nausea so that’s been a welcome change. Though it’s Sophie’s choice, right, would you rather be in pain or nauseous?
She’s prescribed Zofran (for daytime as it’s non-drowsy) and Compazine (for night-time as it makes you drowsy). She was feeling really jittery for the first few weeks of chemo and thought that was a chemo side effect, but it was actually a side effect of Compazine. Once she stopped taking that at night the jitters went away. She was also given Ativan for nausea as an “in case of emergency” kind of drug. She doesn’t like taking it because she doesn’t want to feel “high.”
By week three of chemo she basically went off her anti-cancer diet and started eating whatever she could keep down—this was mostly bananas, yogurt, and bread.
Here are some home remedies and food that helped when the nausea was really bad:
Frequent, small meals
Ginger ale
Ginger tea from David’s Tea
Morning Sickness Tea from the Herb Shoppe
I hand-ground fresh ginger and kept that in the fridge to make tea with
Really uncomplicated foods: Boring chicken breasts, pasta with butter and a little bit of garlic, I made a bunch of congee (she liked it once but can’t do leftovers when she’s nauseous), french toast, pancakes, bananas cooked in butter as a treat
Ensure is a good meal replacement, and was okayed by her doctor (because of the vitamin/supplement content we had to run it by her oncologist)
Edibles and other forms of medical marijuana have helped with the nausea sometimes, but as I’ve said earlier she doesn’t like feeling “high.” A friend gave her a tincture, which is helpful because she can regulate how much she gets (rather than guessing how much to eat of a brownie, right?) and I’ve heard of a different tincture of CBD that doesn’t get you high but is hard to get in New York.
The nausea is better these days but she still experiences it now and again (a couple times a dayish) on the Taxol.
Constipation
This has been an ongoing issue for the last few weeks and it gets really bad. Constipation makes you grumpy and I can definitely tell in her mood if she’s stopped up. It’s also painful and makes her nauseous. Here’s a variety of stuff that helps, sometimes helps, or has been suggested:
Miralax (powder dissolved in liquid, her doctor suggested)
Senekott (vegetable-based stool softener and laxative, Erin the chemo nurse suggested)
Dulcolax (stool softener, Sarah the chemo nurse suggested)
Food remedies we’ve tried:
Prune juice, prunes on her cereal
Fibery cereals
Eating salads
Blueberry/kale involved smoothies (which I make and usually drink, too, and work very well on me)—my recipe is 3 huge handfuls of kale, 1-2 handfuls of spinach, a small handfull of cabbage, enough almond milk to blend the greens comfortably, then I add 1-2 tbsp of brown rice protein powder, 1 small banana, 1 handful frozen blueberries, blend and drink.
Exercising helps relieve the pressure of the gas inside her and last night I had her do a yoga series I’ve done before to move the digestion, which helped move her gas a little. It’s where you lay on the floor, pull up your left knee with right leg straight, hold for 1-2 minutes, switch to your right knee up and left leg straight, hold 1-2 minutes, then do both knees up 1-2 minutes.
She got so constipated before her second infusion of Taxol that she ended up puking after she got the benadryl pre-med! Sometimes after she finally gets relief from constipation she gets diarrhea for a couple of days and finding the happy medium between the two is rough.
Watching her suffer through this I definitely have been feeling a lot of gratitude for my own movements. Anyone out there reading this who has had a normal feeling poo today, send up a little thank you.
Pain
For the bone pain caused by the Neulasta shot, her practice nurse suggested taking Claritin the day before, day of and day after the shot. It has really helped but not gotten rid of the pain entirely.
She’s had a lot of pain from the Taxol. She sometimes gets relief from ibuprophin—600mg helps her with pain, 800mg helps her go to sleep. She has gone to a vicodin here and there but it is constipating and she feels “high” on it so she doesn’t like it as much. Edibles helped once with her pain but the other day definitely didn’t help the pain.
Dara has found that moving around when she can helps relieve the pain and discomfort. Her doctor has said exercising is great when she can do it and she tries to but it doesn’t always feel possible because of her fatigue. Low-impact walks around the block help, dancing to music for four songs is fun, she likes working out at the empty gym in her friends’ fancy apartment building, and doing stretches. I think anyone who has a yoga practice going into chemo is going to be in a good space for relief opportunities.
Massage has been a huge help with joint pain during the Taxol treatment. I’ll often massage her hamstrings, knees and ankles before she goes to bed. I have heard you shouldn’t massage a cancer patient with metastatic cancer (cancer that has spread throughout the body) because it can help move the cancer, so I would definitely check with a doctor before doing that.
At the okay of her doctor she’s been taking calcium and glucosamine/msm supplements to strengthen her joints (helping her joint pain) and strengthening her bones that might be weakened from the chemo. It violates the rules against supplements, which is why she needed to get the okay from her doctor.
 She got this amazing alien design in her hair courtesy of Camera Ready Kutz!
She got this amazing alien design in her hair courtesy of Camera Ready Kutz!
Emotions
Her emotions are so intense right now! She cried real tears at the end of Turbo, the snail movie. She cried real tears during that Macklemore “Same Love” song even though she feels complicated about the institution of marriage.
She finds her emotions are easily influenced, so she cultivates what she watches very intentionally—happy videos, movies and tv shows have been really helpful. (She never watched TV shows before, being mostly focused on work and her social life, so now she’s found all 6 seasons of Parks and Rec and we recently discovered Broad City on Comedy Central.)
She is very strict about only having positivity around her and has had to ask some Debbie Downers to not be negative in their interactions.
She also tries to be real, and sometimes (like yesterday, talking about our first visit to the radiation oncologist) says, “Okay, I just need to vent so I don’t want any bright sides brought up right now.” She’s gotten angry sometimes, and has a few songs about how much chemo sucks. Letting out the negative emotions is just as important as cultivating the positive ones. I do my best to coach her through that as I’ve done a lot of work in that arena on myself.
We’ve been going to the Brooklyn Botanic Garden and just getting into nature a little bit really helps her mood. I read somewhere that fifteen minutes in nature is a huge stress relief. Even when she’s too tired to walk too far, we’ve just gone and lied under a cherry blossom tree.
A simple change of scenery helps a lot, even if she’s not sure she’s up for it, trying something/anything helps (and sometimes if she doesn’t think she’s up for it trying it still helps). We sometimes just go for drives in the car—on Sunday she drove me to Trader Joe’s and sat in the car while I went inside. She didn’t have the energy to help with shopping but being “out” in the sunshine helped her mood tremendously.
Having buddies to talk to has helped. She’s got a couple of people who started chemo after her she talks to and she’s appreciated chatting with other folks about their experiences with similar chemo treatment. I know there are support groups out there and she’s thought about going to one after chemo is over.
She also sees her friends when she can, and we’ve spent some time apart here and there, which I’ll talk about in the caregiving post.
My dog Macy has been a helpful emotional support animal, Dara feels very calm when she sits with Macy on her lap.
Spirituality is a big part of our relationship and both of our lives. We pray before each infusion and pray over the side effects often. It helps to feel spiritually connected.
Hair Loss
She shaved her head so her hair wouldn’t fall out in great clumps. We were surprised at how long it took for it to go away. It was kind of scary while it was happening because there was no way to predict how quickly it would fall out, but now I’m so used to how she looks bald it feels like one of the more insignificant parts of her cancer treatment. She’s also not entirely bald—she still has some “fuzzies” hanging on, maybe about 10% of her hair is left.
By the way, she lost body hair first. Her pubes thinned out, then her chin hairs fell out, then her head. On the Taxol she has thinned out her leg hair and lost some eyelashes. Nothing has grown back.
Other stuff
Her skin feels like it’s crawling sometimes and she has the sense she can feel her organs moving. It’s a weird hypersensitivity and dis-ease feeling.
Chemo brain is a thing! She gets confused sometimes and her already hilariously bad memory gets worse. It’s been less true on the Taxol than the A/C treatment.
Her teeth are getting kind of brown. I heard a lot of folks talking about how important it is to go to the dentist right before and right after chemo in case the chemo has eroded the teeth. A couple of friends told me about people where all their teeth fell out after chemo, totally scary to hear. Here’s hoping everything is okay dentally and otherwise afterward.
Your mouth is like the fastest generating part of your body. Like the cells just reproduce like mad in there, so if you get a nick during regular life you heal overnight but during chemo it doesn’t heal and becomes a sore. To prevent mouth sores you can do this solution of .5 liter of water and 1 tsp each of baking soda and salt. Swish with this 6-10 times a day (basically anytime you eat) and it helps prevent them. Dara got a wicked mouth sore the first week of chemo and her doctor prescribed a topical cream to solve it, but before it went away all she could eat was yogurt.
Little comforts help, like getting a couple of caps for her to wear and cozy jammies. She bought a couple of wigs for work (she freelances so she wears them for client meetings).
Sex has absolutely been affected. I’d say if when she’s healthy we’re at 100%, right now we’re at a 25%? And that’s mostly her just giving one for the team if you know what I mean. Her sex drive has definitely been affected. I’ve found, though, that we find lots of ways to connect the way we used to use sex, so cuddling, being intimate otherwise and creative helps.
I am Reiki Level One certified (getting Level Two this weekend) and have been doing reiki treatments on her here and there and they seem to help. My instructor said that his friend with breast cancer liked getting treatments right before her chemo infusions, but I think it depends on when the person wants to have that kind of energy.
A friend suggested the book The Chemotherapy Survival Guide and that’s been really helpful as a reference guide.
Asking questions is totally my MO—I like to ask questions until I really understand things. So I’ve learned a lot about chemo. There’s never a perfect permutation for how to deal with chemo side effects, you just kind of throw stuff at it until something works.
I hope some of this helps anyone out there going through chemo or who has a loved one going through chemo and you want to understand it better. I genuinely hope that Dara is “one and done” with chemo and with cancer.
I’ll be back with a couple of other posts about the experience, and my Instagram has been basically a live blog of the experience of breast cancer. Dara has a great vlog about what she’s been learning from her cancer experience.




Thank you for sharing this so honestly. My step father is going through chemo at the moment for non Hodgkins Lymphoma and information seems to much sketchier here in the UK than in the US. I didn’t know for example that you can’t take vitamins on chemo. I will make sure my mum knows this. I wish you and Dara the best of the best.
I LOVE that you shared all of this, and with so much wit and compassion. I have a loved one who just went through chemo, but he didn’t survive his very aggressive kind of cancer. :'( I am grateful to you for just laying it all out there, likely not only because it was helpful for you but also so it could be helpful to others. Thanks.
I thoroughly enjoyed your blog about Dara’s experience with chemotherapy. I’m currently receiving chemotherapy and I found relief in knowing I’m not the only one experiencing these crazy side effects. I hate she had to go through this, but reading her story has helped me to see this rollercoaster is doable and it’s OK to cry. I find myself trying to be strong, but I have days I just want to kick and scream. Doesn’t help I have 3 children ranging in ages one to fourteen that are watching my every move. I’m almost finished with my A/C treatment and I have already completed 12 weeks of taxol and carboplatin. I find it helpful to read about women who have gone through this before me. In some weird way it validates my feelings during treatment and helps me to see the light at the end of the tunnel.
I’m so glad it was helpful for you, Melissa!! Being gentle with yourself is so important! I wish you all the best of luck getting through chemo and getting to cancer free!!!